Comprehensive Mental Health Billing | made by doctors for doctors
- doctor for doctor service
- lowest claim denials
- lowest percentage in the USA
mental health billing services made by doctors to serve doctors
Welcome to RGTrend, where we specialize in mental health billing services designed to simplify reimbursement processes, reduce administrative strain, and help you stay compliant with industry regulations. Our team combines experience in mental health coding, expertise in insurance claims, authoritativeness through proven case studies, and trustworthiness by adhering to HIPAA standards—ensuring your practice remains efficient, profitable, and patient-focused.

Dedicated Team of Specialists:
Our mental health billing specialist experts are medical doctors who have in-depth knowledge of psychiatric, psychotherapy, and behavioral health nuances.
Compliance & Security:
- We follow mental health billing guidelines & HIPAA compliance rules rigorously, backed by secure data handling and encryption practices.
- HIPAA Adherence: At RGTrend, safeguarding PHI (Protected Health Information) remains a top priority. Our systems meet and exceed HIPAA standards.
End-to-End Support:
From verification of benefits to claims submission and follow-up, we handle the mental health medical billing process comprehensively.
our pricing: Transparent medical billing Cost Structure, no additional fees:
We know mental health billing services cost is a concern. That’s why we provide clear, upfront pricing options so you can budget with confidence.
Proven Results:
Through billing compliance and regulations best practices, we consistently minimize denials, shorten payment cycles, and boost revenue for mental health professionals.
dedicated department
to support your practice and answer your questions anytime, making sure your mental health practice keeps growing
Understanding the Complexity of Mental Health Billing
Providing quality care for mental health patients involves unique challenges—both clinically and administratively. Insurance companies often apply strict policies for coverage, documentation requirements differ from other specialties, and coding and billing for mental health services can become complicated fast.
At RGTrend, our mental health billing services go beyond merely submitting claims. We address every aspect, from verifying patients’ mental health coverage to accurately applying mental health billing codes and billing codes for mental health services. By integrating electronic medical billing software and electronic health records (EHR) integration, we streamline workflows so clinicians can focus on providing excellent care rather than drowning in paperwork.
Key Subspecialties We Support
Our mental health billing services cover the full range of mental health sub-disciplines. Each specialty faces unique billing hurdles, and we tailor our process accordingly:
Psychiatry Medical Billing Services
Psychiatrists often handle both therapy and medication management. Our psychiatry medical billing services ensure you navigate insurer requirements for medication visits, therapy sessions, and any additional evaluations. We also offer psychiatric billing services to accommodate differing scopes of psychiatric care.
Psychology Billing Services
With psychology billing services we handle everything from testing and evaluation codes to therapy session claims. Psychological testing often requires more detailed documentation—our team makes sure you stay compliant while maximizing reimbursements.
Billing Services for Therapists
Clinical social workers, marriage and family therapists, and licensed professional counselors all benefit from RGTrend’s billing services for therapists. We cater to each profession’s specific documentation and coding demands. Our specialized knowledge of mental health billing guidelines & HIPAA compliance helps reduce denials and keep your revenue cycle healthy.
also social work and behavioral health and more, Our billing and coding services cover the full range of mental health sub-disciplines.
Our
Approach to Mental Health Medical Billing: this helps us reduce claim denials and ensure accuracy and hippa compliance
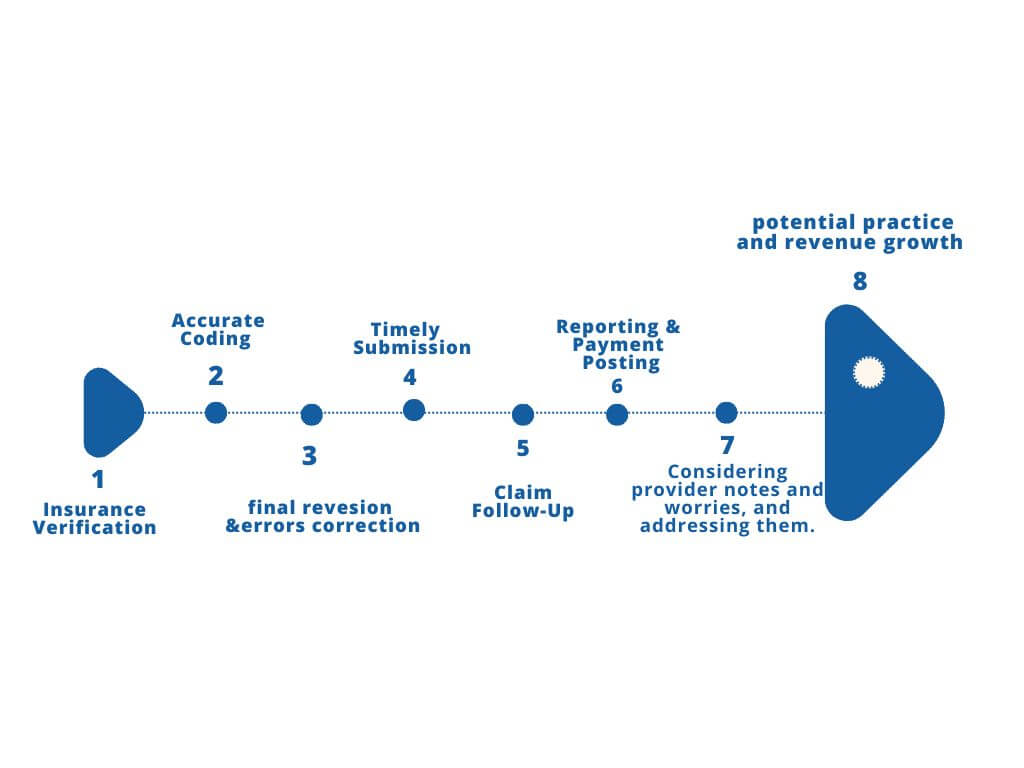
Insurance Verification for mental health billing
AAPC-Certified Specialists: Our billing team includes AAPC-certified professionals who understand the nuances of mental health coverage requirements. Real-Time Eligibility Checks: We access payer portals to verify copays, deductibles, session limits, and pre-authorization needs for diagnoses like Major Depressive Disorder (F32.0, F32.1) or Generalized Anxiety Disorder (F41.1). Why It Matters? By confirming benefits upfront, we drastically reduce denials and ensure patients know their out-of-pocket responsibilities before therapy begins.
Accurate Coding adn Use of Mental Health ICD-10 Codes
Use of Mental Health ICD-10 Codes: We apply precise ICD-10-CM codes—e.g., F32.0 (Major Depressive Disorder, single episode, mild) or F43.2 (Adjustment Disorders)—to reflect each patient’s clinical presentation. DSM-5 Alignment: Our coders cross-reference DSM-5 criteria with ICD-10 codes, ensuring each claim accurately represents the patient’s diagnosis and treatment. Why It Matters? Proper coding is critical for timely reimbursements and compliance. Insurers often deny or delay claims with missing or incorrect codes. Our specialized knowledge of mental health coding prevents costly mistakes.
Claim Final Revision & Errors Correction
- Multi-Level Checks: Our senior billers review each claim one final time—verifying proper CPT codes for psychotherapy (e.g., 90834 for 45-minute sessions) or psychiatric diagnostic evaluations (e.g., 90791), as well as the mental health ICD-10 codes.
- Adherence to Payer Guidelines: We stay current with the CMS mental health services billing guide2025, making sure every submission meets payer-specific documentation rules.
- Why It Matters:
A thorough pre-submission review dramatically lowers denial rates, saving you time on appeals and helping you get paid faster.
Timely Submission
- Electronic Claims Integration: We sync seamlessly with your Electronic Health Records (EHR) integration to minimize manual data entry.
- Rapid Turnaround: Claims are typically submitted within 24–48 hours after your documentation is finalized, speeding up the reimbursement cycle.
Why It Matters:
Prompt submissions reduce cash-flow disruptions and demonstrate to payers that your practice meets administrative standards.
Claim Follow-Up
- Dedicated Account Managers: Each practice works with a single point of contact who monitors claim statuses, flags potential issues, and communicates directly with payers.
- Appeals & Denial Management: If a claim is denied—perhaps because of missing modifiers or insufficient documentation—we handle appeals swiftly, providing any additional clinical notes needed.
Why It Matters:
Timely follow-up ensures that underpaid or denied claims don’t linger unaddressed, maximizing your revenue potential.
Reporting & Payment Posting
- Transparent Monthly Reports: Our system generates clear, itemized statements showing which claims are paid, pending, or denied—along with specific denial reasons.
- Compliance & Confidentiality: Payment data is stored using HIPAA-compliant security measures, and staff undergo regular training to maintain patient confidentiality.
Why It Matters:
Accurate payment posting and transparent reporting give you a real-time snapshot of financial health, enabling better practice management decisions.
Considering Provider Notes & Worries and addressing them
- Proactive Communication: We invite therapists, counselors, or psychiatrists to share specific concerns (e.g., unique therapy modalities or specialized testing codes).
- Clinical Documentation Support: Where needed, we advise on best practices for chart notes that align with ICD-10 diagnosis requirements—important for borderline cases like F41.1 (Generalized Anxiety Disorder) vs. F41.9 (Anxiety Disorder, Unspecified).
Why It Matters:
Your clinical expertise is the foundation of each claim. By listening to your input and clarifying any ambiguities, we strengthen the accuracy of both coding and billing.
Potential Practice & Revenue Growth | at rgt we understand that your growth=rgt growth
.
- Future-Proofing: We track emerging regulations in mental health billing—particularly updates to mental health billing codes 2025—so your practice is always prepared.
- Strategic Consultation: Our billing analytics help identify high-revenue services or potential expansions—e.g., adding group therapy sessions or specialized testing—based on payer data trends.
Why It Matters:
When your billing cycle runs smoothly, you can devote more energy to patient care, expand your service offerings, and ultimately achieve greater financial stability.
By integrating clinical insight, regulatory compliance, and cutting-edge billing expertise, our custom approach to the mental health medical billing process ensures that every claim is filed accurately and on time—so you can focus on what you do best: providing exceptional mental health care.
Transparent Mental Health Billing Services Cost
We understand that mental health billing services cost is a key factor for many practices. RGTrend offers multiple pricing models—percentage-based or flat-rate—depending on your practice size, volume, and complexity. Our transparent approach gives you a clear picture of monthly expenses without surprise fees. Ultimately, we aim to provide a cost-effective solution that balances affordability with top-tier service.
Case Study: Boosting Revenue for a Group Therapy Practice
Dr. Smith, a clinical psychologist managing a group therapy clinic, struggled with high claim denials and slow reimbursements. Within three months of switching to RGTrend’s mental health billing services:
- Denial Rate Decreased by 40%.
- Average Reimbursement Time improved from 45 days to under 25 days.
- Patient Satisfaction increased due to transparent billing communication.
This success story is just one example of how our mental health billing services can transform your revenue cycle.
Frequently Asked Questions about mental health billing :
How do I bill Medicare for mental health services?
Billing Medicare requires strict adherence to coverage guidelines, including session limits and documentation. We help verify eligibility, apply the right mental health billing codes, and submit all required forms for you.
How much does a mental health billing service charge?
Mental health billing services cost depends on your practice size, payer mix, and service level. We offer flexible pricing structures—percentage or flat rate—to match your needs.
How to bill Medicare for mental health services?
Our mental health billing specialist verifies your patient’s specific plan details, obtains any necessary authorization, and submits accurate claims with correct modifiers and codes. We stay updated on the cms mental health services billing guide2025 to ensure compliance.
How is mental health billing different from medical billing?
Coding and billing for mental health services can involve varying session lengths, therapy types, and confidentiality requirements. This specialized approach contrasts with more standardized medical billing codes.
How to bill for mental health services?
Proper billing starts with correct patient intake and insurance verification. Then, accurate documentation of each session—combined with timely electronic submission—ensures faster reimbursement. Our mental health billing services handle all these tasks so you can focus on patient care.
Testimonials
Ready to Elevate Your mental health Practice?
Whether you’re a solo therapist or a large psychiatric clinic, our mental health billing services are custom-built to suit your needs. Enjoy better reimbursement rates, compliance peace of mind, and more time for patient care.
Let us show you how RGTrend’s specialized approach to mental health billing approach can boost your practice’s efficiency and revenue.
Additional Resources related to mental health billing
Contact us now to explore how our mental health billing services can help you see higher reimbursements(up to 20% difference which we have done with our doctors before ), simplified administration, and more time for patient care.
